Miriam Pérez Vallmitjana and Ignacio Ginebreda Martí
ABSTRACT
For more than 30 years, psychological support has been provided by our department to all patients affected by skeletal dysplasia and congenital malformations who must undergo surgical procedures for bone elongation and bone or joint corrections.
The methods applied and the evaluation of the follow-ups during the procedures and at the end of the same are described here. It shows that the preparation and psychological support of this type of patients is of great importance. This is done by sitting in on medical visits, giving advice as well as advocating for the early detection of complications and resolution of any problems.
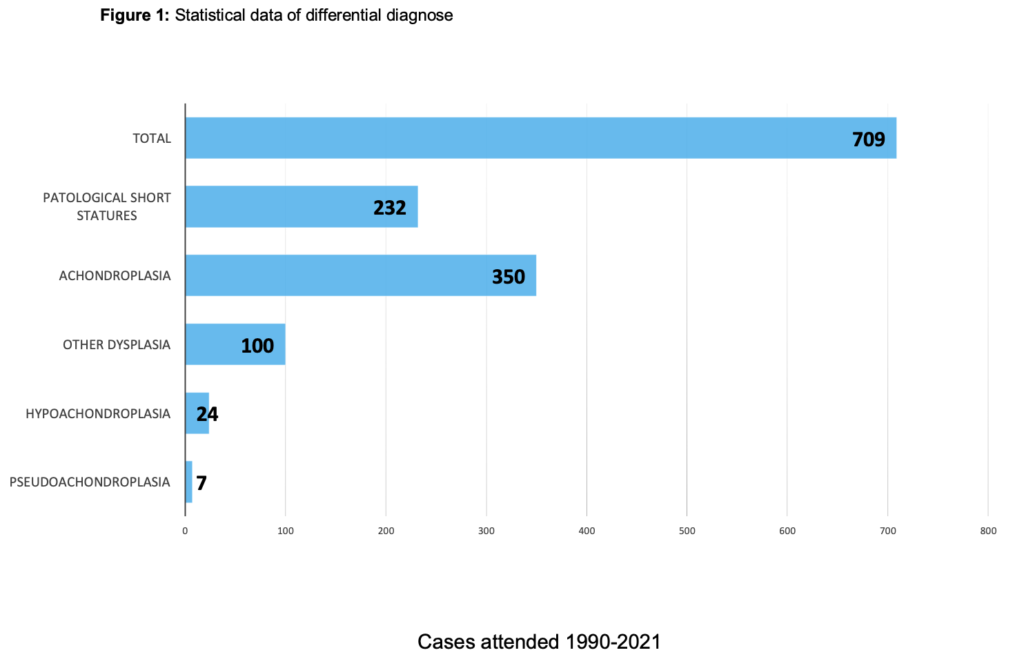
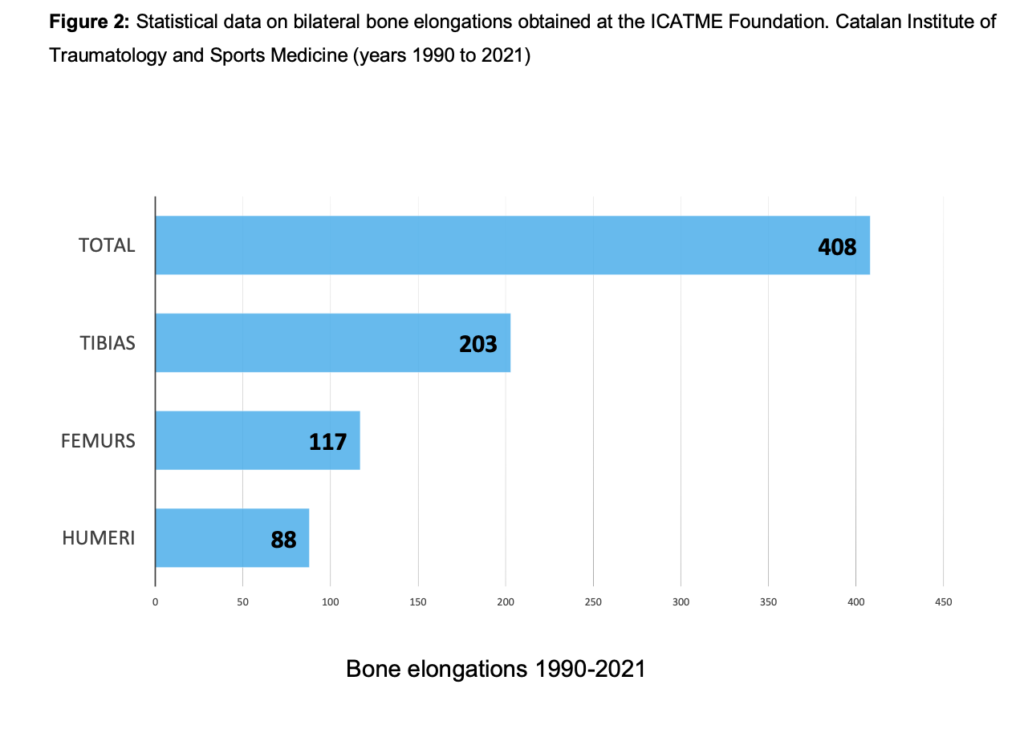
Methods: Between 1990 and 2021, 709 patients diagnosed with achondroplasia, skeletal dysplasia, and pathological short stature were treated. Moreover, 408 bilateral bone elongation surgeries were performed.
Results: After more than 30 years of experience, it has been determined that there is a low rate of complications when providing psychological support in the care of patients with bone dysplasia and to those undergoing bone elongation procedures. The psychological preparation and the collaboration of the patient and their parents with the aid of the medical team are decisive factors in obtaining optimal results with this type of treatment.
Conclusions: Given the characteristics of patients with skeletal dysplasia, psychological help is included as a necessary support in multidisciplinary care.
INTRODUCTION
Achondroplasia is the most common Osteochondrodysplasia that results in short stature. It is commonly denominated dwarfism and occurs in 1 in 25,000 live births.2 It is due to mutations in the Fibroblast growth factor receptor 3 (FGFR3) and is most often a spontaneous autosomal dominant inherited mutation.2 That mutation causes a congenital defect that affects skeletal growth. Consequentially, it produces a disproportion between the trunk and the extremities as well as a characteristic physiognomy. The final height prognostic is approximately 124cm in women and 130cm in men.2
People with achondroplasia exhibit normal intelligence and short stature with various skeletal abnormalities along with other associated problems.3
After more than 30 years of experience in the Growth Pathology and Bone Elongation Unit, people affected by achondroplasia, other skeletal dysplasias and growth pathologies have been seen to present a series of special psychological characteristics that must be treated in multidisciplinary units dedicated to their care. Individual psychological interviews, interviews with parents and psychological preparation for surgical interventions are essential to the good evolution of long-term surgical procedures like limb-lengthening.
METHODS
Between 1990 and 2021, 709 patients with growth pathologies (mostly achondroplasia) were treated and 408 extremity elongation surgeries were performed.
Below is a table with the data on the different pathologies treated.
Psychological support was provided by sitting in on medical visits, through individual and family psychological interviews, and aiding in psychological preparation prior to surgical interventions. Likewise, the follow-up, coordination and management of the case was done. The specific tasks of giving psychological support and the coordination and management of the case were always carried out by the same assigned professional.
1. Growth Pathology Unit Specialized in Achondroplasia
Boys and girls with achondroplasia present psychological aspects that, in parallel to the physical ones, must be addressed.
The professional team takes care of providing all possible information and helping parents in the process of accepting the diagnosis.
Psychological interviews help them to express feelings and not deny the emotions of the affected person and their parents in their coming to terms with their circumstance.
These acceptance processes are one of the main aspects that are promoted from the psychological angle in the Growth Pathology Unit of our center. It was one of the reasons the work with groups of patients began.
Currently, a presumptive diagnosis of achondroplasia can be obtained by means of ultrasound around the seventh month of pregnancy. To confirm the diagnosis, a molecular genetic study is performed shortly after birth.
During the first years of life, development is slower than normal, and it is necessary to carry out a specific medical follow-up with diagnostic tests. The potential health problems derived from achondroplasia must be suspected and taken into account3. They include foramen magnum stenosis, muscle hypotonia and hearing loss due to frequent incidences of otitis (and the need for drainage surgery).
In children with achondroplasia, walking and language acquisition are consolidated one or two years later than expected for their age. They also present with difficulties like delayed development of psychomotor skills. Parents are often called to use the child stroller until they are 3-4 years old and help their child with hygiene until they are 8-9 years old. They will also have to adapt the furniture in the house to promote autonomy and avoid frequent falls. These situations cause great concern and lead to the child being perceived, by the parents, as smaller and more fragile than other children.
When the very children affected by achondroplasia begin to come to terms with their condition, it is difficult for them to understand their differences and accept their own body image.
Feelings of inferiority and low self-esteem brought on by fear of rejection, ridicule and discriminatory treatment may arise. All this comes together with the social stigma that is implicit in having skeletal dysplasia, short stature or dwarfism.
In parents, the appearance of defense mechanisms like overprotection and denial of the problem is common. It is important to restrain oneself from such reactions since they may contribute to psychological problems like insecurity, emotional isolation, excessive family dependency, a lack of autonomy and difficulties in the developing self-reliance in the person with achondroplasia. Nowadays, families better accept achondroplasia than years ago.
It is recognized that the strength of the bond established between the parent/s and the child is the most decisive factor in their acceptance of their condition, in the formation of character and in the level of self-esteem and autonomy of the child.4
Bone elongation surgical interventions: The emotional and psychological impact
The ICATME bone elongation technique with monolateral external fixators for patients with achondroplasia was described by Vilarrubias et al. in 19905.
The statistical data on the bilateral bone elongations performed between 1990 and 2021 are presented below. (Fig. 2)
The global limb lengthening program begins between the ages of 10 and 12 and consists, firstly, of the tibiae lengthening surgery, and then that of the femurs and humeri.6
Upon completion of the elongation program, a height of around 150cm is achieved, assuming an elongation of 15cm in the tibias, 13-15cm in the femurs and 8-10cm in the humeri.7
Bone lengthening processes are long-term treatments of about one year. Patients have to carry out the lengthening, the healing of the fixator nails and a specific rehabilitation program on a daily basis. During most of the stretching of the tibiae and femurs, they will use a wheelchair with a platform and keep their legs stretched.
Great importance is attached to informing the patient and their parents about the entire surgical process, as well as the expected results and the risk of complications. In this line of work, it is of great value for patients to meet other patients in the same situation.
It is necessary to insist on carrying on with a normal life, studies and school attendance to keep up academic activities and foster relationships within the peer group.
Surgical treatment can be started when the ideal conditions exist. In cases of other types of skeletal dysplasia8, the follow-up and a type of surgical intervention is carried out based on an individualized study of each case.
Bone elongations should be performed in multidisciplinary units with specialized professionals who can provide adequate medical and psychological monitoring.
Bone lengthening can be perceived as the solution to short stature and its psychological and social implications, but the changes to which one’s body image would be subjected can lead to an emotional imbalance that is important to be alert to at the psychological level.
It is also important to be aware that the beginning of the lengthening process coincides with pre-adolescence, a key stage for the consolidation of identity and an appreciation of one’s own body.
2. Psychological Assistance
Psychological preparation
In 1989, a surgical psychoprophylaxis project was started with the aim of preparing boys and girls with achondroplasia for surgical lengthening procedures and to help the doctor and the family in the face of any difficulties that might arise.
With psychological support, they can better reflect on their options and make the right decisions for them in the face of a complex life-changing situation, be it either short stature or skeletal dysplasia. For this professional help to be effective, it is necessary to get to know of the boy or girl, their degree of maturity, interests and motivations and the type of family and its dynamics.
In 1994, with the creation of the Growth Pathology Unit, psychological care was integrated into the medical team. That made it possible to improve the psychological preparation for interventions and offer broad care to the patient and family.
Objectives of psychological interviews for patients
- Evaluate the level of understanding, difficulties, interests and abilities through graphic projective techniques and non-directed interviews.
- Know the academic and social level (adaptation to the class group, social and family relationships).
- Assess the motivation, fantasies and fears in front of the intervention to adapt expectations to reality.
- Propose, as a prerequisite for interventions, contact with patients in a similar circumstance and their parents.
- Prepare the boy or girl for the intervention (surgical psychoprophylaxis) by helping to manage anxiety, fears and uncertainties before the operation and the hospital stay.
- Establish a relationship of trust and collaboration and follow-up during and after the surgical process.
Objectives of psychological interviews for parents
- Know family dynamics and personal and socioeconomic resources. Look at how the parents have dealt with the diagnosis and determine the type of bond established between them and the affected child.
- Establish a therapeutic alliance and make a commitment to collaborate with the patient and their parents.
- Encourage and give value to the healthy aspects of the family to improve the prognosis of the operation.
- Promote acceptance of the diagnosis to help avoid denial and overprotection.
- Propose meeting with other families through visits, family days and parent groups.
The presence of psychopathologies in the child or an unstructured family style are risk factors for intervention3, and it is important to evaluate them beforehand. The Growth Pathology Unit established an action protocol listing possible contraindications for bone elongations. The information obtained in the psychological interviews helps to assess the case and outline the indication for surgical intervention.
In the interviews, a space is established to promote individual thought and reflection. Much importance is attached to the fact that it is the child-patient who makes the decision to undergo surgery, the one who knows the implications and that the decision has been agreed upon and discussed with the parents.
At a psychological level, the containment of anxieties and the build-up of fears are very important aspects to manage. It is also imperative to assure that the child is well informed and kept in the company of the parents over the longest period possible up to the surgical procedure.
Below are 2 cases with fictitious names to illustrate the psychological interviews with children.
Maria, 12 years-old: achondroplasia
Psychological interview prior to tibia lengthening. Free drawing. Indicated intervention.
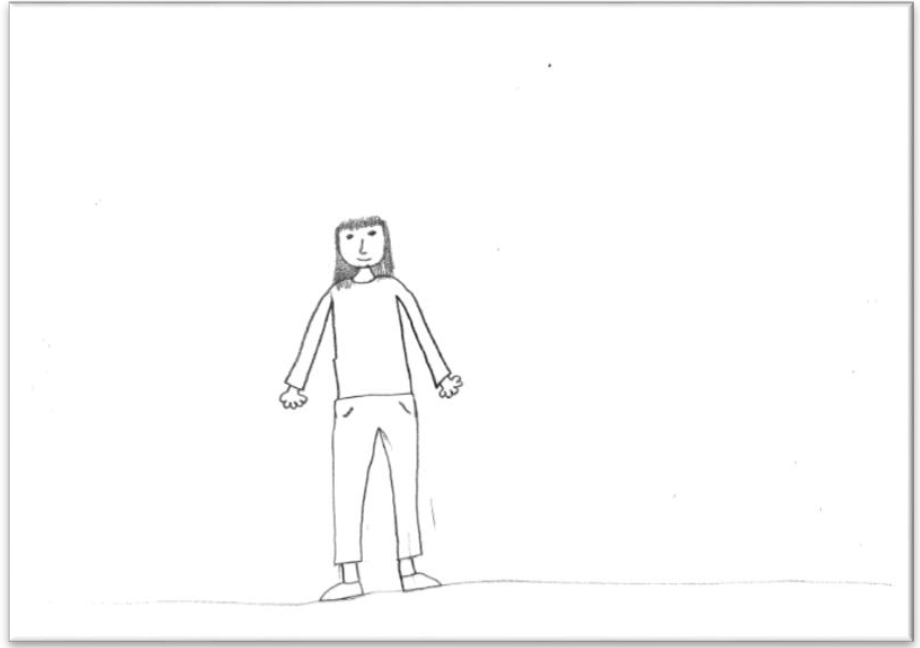
There are no contraindications present. She has a good school level, realistic expectations, good family organization and sees lengthening as added value for her physical and personal growth. There is a consensus among all the stakeholders with regard to the medical indication.
Text written by the mother of Maria:
“Achondroplasia has a physical aspect that is treated by traumatologists and other specialists. It also has an emotional aspect for both the affected person and his/her family and psychologists deal with that aspect. For us, it is very important since emotional accompaniment is very necessary. Since María was 2 years old, she has been visited in the unit and the parent meetings are a great support”.
María is currently going to high school, with good results, while undergoing the process of humerus lengthening.
She previously underwent the tibiae and femurs elongation procedures. She is now 150cm tall. Next year, she plans to start university studies.
Oscar, 15 years-old: Bone dysplasia
Follow-up visit. Free drawing. Has learning difficulties.
Intervention contraindicated. The patient lacks interests in an intervention. Intervention contraindicated due to present degree of psychological emotional development. Annual follow-up visits will be conducted.

Coordination and case management
In 2003, an agreement was established between the GPU (Growth Pathology Unit) and the Department of Health of Catalonia (Cat-Salut). The GPU is a reference unit specializing in the care and treatment of achondroplasia, other dysplasia types and growth disorders9.
With this agreement, the psychological support integrated into the unit has been favorable for its validation and continuity
3. Work with Groups
People of all ages with skeletal dysplasia can find themselves with feelings of loneliness, social isolation and even deny the problem exists. They also experience difficulties in obtaining resources and responsibly deciding on medical treatments.
The work carried out at ICATME with groups of patients and their families is very important in addressing these aspects and constitutes an institutional resource of great value.
In 1995, meetings for the parents of boys and girls with achondroplasia began. This space has allowed for the exchange of family experiences and information on the extension processes and has facilitated the establishment of friendships and nurtured a mutual support network.
The first Families and Professionals of the Unit Day was held In the year 2000. This periodically repeated event has also constituted an opportunity for information gathering and communication among the affected people.
In 2009, the care for adults with skeletal dysplasia program was consolidated and group meetings began to work on its psychosocial aspects and offer comprehensive care. The objectives consist of promoting personal autonomy and self-reliance, developing interpersonal relationships and responsibility for one’s own health.3
Given the observable benefits in these meetings and the demand of the patients, the Theater workshop for adults with skeletal dysplasia began in 2015 with the aim of building greater self-esteem and forging group cohesion.
New friendships have been made and others consolidated and group events are currently organized of a group that did not have this type of activity. In 2019, the Art Therapy Workshop for adolescents in the process of elongation and for those young people who had already undergone the process was created. It is about promoting personal autonomy, increasing motivation in the area of academics and training for work, having a reference group and building a life project.
RESULTS
Psychological assistance is included in the multidisciplinary Growth Pathology Unit. After more than 30 years of experience, it is affirmed that the functions of psychological support and case management are essential, especially when a surgical intervention must be decided and during the rehabilitation period.3
The presence of psychological support means better management of incidents during the bone elongation processes, since the collaboration of the patient and their parents is decisive for a satisfactory result.10.
This psychological care included in the multidisciplinary unit is what allows us, from the community health model, to offer comprehensive medical care based on a strong-positive relationship with the patient.
The characteristics of the unit are those that are included in the guidelines stipulated for the treatment of rare diseases.
DISCUSSION
People with skeletal dysplasia are a vulnerable population group that experiences discrimination, rejection and emotional difficulties. Based on the experience of the growth unit, we believe that comprehensive care that includes psychological support is necessary.
Patients are offered specialized medical and psychological monitoring and group cohesion activities to improve their quality of life throughout their lives.
Case management and psychological support are considered essential in the coordination and guidance of people affected by rare diseases with a multipathology convergence.
To improve care for patients with skeletal dysplasia who must face complex surgical interventions throughout their lives, specific tools would be necessary. Moreover, there is a need for agreement on the most useful types of psychological assessment and health-related quality-of-life tests called for to meet the needs of those people.
The SAR-Covid 19 pandemic has had a significant impact on the care of patients with skeletal dysplasia. As well, it has caused greater isolation, a general situation among those with rare diseases and other vulnerable collectives.
BIBLIOGRAPHY
1. Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990 Jan;(250):81-104. PMID: 2403498.
2. Orphanet Encyclopedia of Disability. (2017). Achondroplasia (online). Orphanet- Spain day. Available in:
https://www.orpha.net/data/patho/Han/Int/es/Acondroplasia_Es_es_HAN_ORP HA15.pdf.
3. Santana Ortega, A.T. & Castro Hernández J.J (2008). Achondroplasia, more than just a question of height. Las Palmas de Gran Canaria: Family Association of People Affected by Achondroplasia (AFAPA), University of Las Palmas de Gran Canaria (ULPGC). Available in: https://www.fundacionalpe.org/images/library/a.pdf
4. Coderch J., & Plaza Espinosa A. (2016). Emotion and Human Relations: Relational Psychoanalysis as Social Therapeutics. Ágora Relacional, S.L (Rational Thought Collection, 15)
5. Vilarrubias, JM., Ginebreda I. y Jimeno E. (1990) Lengthening of the lower limbs and correction of lumbar hyperlordosis in achondroplasia. Clin Orthop Relat Res, (250),143–9.
6. Correa Vázquez, E., Ginebreda Martí, I. and Cáceres Palou, E. (2011). Health- related quality of life in post-lengthening achondroplasic patients. Research Paper, Department of Surgery, Universitat Autònoma de Barcelona, Bellaterra, Barcelona.
7. Ginebreda I, Campillo-Recio D, Cárdenas C, Tapiolas, J, Rovira P, Isart A. (2019). Surgical technique and outcomes for bilateral humeral lengthening for achondroplasia: 26-year experience. Musculoskeletal Surg,103(3), 257-262, doi: 10.1007/ s12306-018-0583-3.
8. Mortier GR, Cohn DH, Cormier- Daire V, Hall C, Krakow D, Mundlos S, Nishimura G, Robertson S, Sangiorgi L, Savarirayan R, Sillence D, Superti-Furga A, Unger S y Warman ML. (2019) Nosology and classification of genetic skeletal disorders: 2019 revision. Am J Med Genet A, 179 (12),2393-2419, doi: 10.1002/ ajmg.a.61366.
9. Solà-Morales, O. & Pons, J. MV.(2003). Evaluation of the clinical need and the structural, technical and human criteria of a reference center for the care of people with achondroplasia. Madrid: Agency for the Evaluation of Medical Technology and Research/Agència d’ Avaluació de Tecnologia i Recerca Mèdiques (CAHTA). Available in:
https://www.fundacionalpe.org/images/alpe/library/societyEN/Evaluacin-de-la- necesidad-clnica-y-de-los-criterios-estructurales.pdf
10. Pombo M. Co-editors (2009). Treatise on Pediatric Endocrinology, 4th edition. McGraw-Hill-Inter-American. Cap 20. Surgical treatment of hypogrowth. Ignacio Ginebreda Martí, José Ma Vilarrubias Guillamet.
PSYCOLOGY PRESENTATIONS
- Pérez Vallmitjana M, 1st Multidisciplinary Symposium on Growth Disorders. “Psychological assistance in the growth unit” Barcelona 1996
- Pérez Vallmitjana M, 4th International Bone Dysplasia Meeting. “Psychological assistance and preparation for extremity elongations”. Baden Baden 1999
- Pérez Vallmitjana M, II International Meeting on Achondroplasia. ALPE Foundation- Achondroplasia. “Psychological assistance in the Growth Pathology Unit”. Gijon. 2002
- Pérez Vallmitjana M, VII National Symposium on Growth: XXI century. National Association for Growth Problems CRECER. “Action protocols of the agreement between the Servei Català de la Salut (Cat-Salut) and the Growth Pathology Unit (ICATME Foundation)” Madrid 2003
- Pérez Vallmitjana M, II Conference on Achondroplasia. Association of small great fighters PEGRAL. Family association of those affected by achondroplasia AFAPA. “Psychological Assistance in the Growth Pathology Unit” Tenerife 2004
- Pérez Vallmitjana M, III International Meeting on Achondroplasia. ALPE- Achondroplasia Foundation. “An experience in Group of Parents” Gijón. 2006
- Pérez Vallmitjana M, XI Symposium National Association CRECER. Socio- sanitary needs of pathological short stature. Table Speaker: “Bone elongation: medical and social controversy”. Madrid 2006
- Pérez Vallmitjana M, XXI National Congress of the Spanish Society of Child and Adolescent Psychiatry and Psychotherapy SEPYPNA. Poster presentation “Psychological assistance in a growth unit” Almagro. 2008
- Pérez Vallmitjana M, XIV SEFEX basic course. Spanish Society of External Fixation. “The importance of psychological preparation in external fixation”. Granollers 2008
- Pérez Vallmitjana M, IV International R+D+i Meeting in Achondroplasia. InnovationDevelopmentResearch. ALPE-Achondroplasia Foundation. 7th table: “From the individual to the group: Psychological coping with social stigmatization.” Gijon 2010
- Pérez Vallmitjana M, V International Congress on achondroplasia. ALPE- Achondroplasia Foundation. “Clinical follow-up in adults with bone dysplasias. Gijon 2014
- Pérez Vallmitjana M, III Conference on bone dysplasias and skeletal anomalies in childhood. “Multidisciplinary care”. Valencia 2018
- Pérez Vallmitjana M, Canu N, XXII Congress of achondroplasia and other growth disorders. National Association for Growth Problems. GROW Presentation: “Protocol of action in adulthood.” Murcia 2021