Skeletal Dysplasias (SD) refer to a group of health conditions characterised by musculoskeletal problems and growth defect in bones, being achondroplasia the most common form of skeletal dysplasias that cause short stature. They are considered rare diseases, as they affect less than one person in 2,000.
What are the causes of SD?
There are multiple medical reasons for skeletal dysplasias, which can be classified in three broad categories: fetal exposure to toxic or infectious elements, hereditary diseases of the skeletal system and, the main one, genetic alteration.
In 2010, a study showed the existence of more than 450 different skeletal dysplasias, of which, 316 were related with mutations in one or more of 226 different genes. Among them, molecular alterations in three genes were responsible for most of the dysplasias: FGFR3, COL2_1 and SHOX.
Achondroplasia, the most common dysplasia, comes from a mutation in the mentioned FGFR3 gene. This genetic mutation appears spontaneously in one of the progenitor cells (without mutations in the parents) in 80% of the cases.
Thus, 90% of children with achondroplasia have no record of the disease in their families.


Diagnosis
Skeletal dysplasias are diagnosed through radiographic, clinical and molecular criteria.
Radiographic detection
Achondroplasia can generally be diagnosed, from the end of the second trimester onwards, by prenatal ultrasound examination.
Most commonly, individuals with SD have certain features that allow the diagnosis through radiographic systems, such as:
- Shortening of long bones with alterations in the shape
- Proximal limb length disproportion
- Excessive curvature of the lower back
- Broad, short and trident-shaped hands
- Macrocephaly
- Frontal bossing, and midface hypoplasia
Nevertheless, bear in mind that a complete certainty in the diagnosis of skeletal dysplasias is always postnatal.

DNA Analysis
Thanks to new scientific developments is possible in some cases to have a prenatal non-invasive diagnosis by analysing cell-free fetal DNA (cffDNA) circulating in maternal blood.
Clinical detection
Some SD conditions can only be detected after birth based on multiple tests.
The importance of early diagnosis
Early diagnosis and the subsequent early intervention are key in order to prevent further health problems arising from early childhood if they are not addressed on time.
- Early intervention is directed to the child population from 0 to 6 years of age and his family. These interventions, which must consider the child as a whole, must be planned by a team of professionals with an interdisciplinary orientation.
- Beyond expert support, the awareness of the child’s own family about the care and needs of the infant is highly important.
The assimilation process
We know that finding out that your son or daughter is born with a SD condition is not easy news. As rare diseases, there is limited information, and can involve a long diagnostic process and lack specific treatment sometimes.
- Each person has a different way to deal with this situation, but it is normal that you face a high level of uncertainty and distress after the diagnosis. It it is ok to be angry, sad and have mixed feelings. It is important not to neglect our own mental health and look for support to make it easier to manage our feelings through the process.
Do you have questions? Join our network...
Health impacts
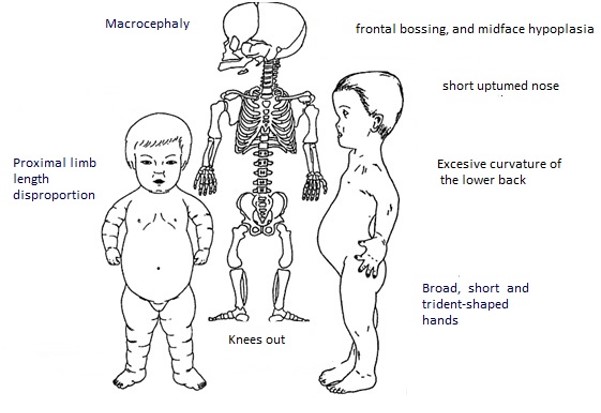
Most commonly, people with SD have features beyond the short stature, such as proximal limb length disproportion, excessive curvature of the lower back, broad, short and trident-shaped hands, macrocephaly, frontal bossing, and midface hypoplasia. All these features can lead to concrete health consequences.
- Hydrocephalus
- Cleft palate
- Scoliosis
- Arthrosis and other skeletal problems
- Neurological affectations
- Auto-immune problems
Some of those need immediate attention during the childhood, whereas others evolve with age. Keep in mind that proper care and regular check-ups will prevent more serious episodes.
Neurological impacts
Patients with DS are at increased risk of neurological complications due to the endochondral ossification of the skull base.
Children with achondroplasia have normal intelligence but may be delayed in motor milestones, due to the particularities of their anatomy, without involvement in other areas of neurodevelopment.
Otorhinolaryngological impacts
Individuals with DS are at increased risk of obstructive apneas. Due to the anatomy of the auditory canal, they are also at greater risk of suffering from otitis during childhood.
Traumatological impacts
Lumbar deviation and varus deformity of the tibia is common (40-70% of patients). This varus deformity can trigger symptoms including mechanical pain and limitation of walking and other physical activities.
Metabolic impacts
Primarily, people with DS are more likely to develop obesity, as a co-morbidity associated with decreased physical activity and decreased basal metabolism.
Treatment
In recent years, learning and research on SD has gradually increased. Noteworthy, work of geneticists on achondroplasia assessing the developmental impacts in children, neurological and respiratory issues, practical and emotional support, and main aspects of transitional care.
Various treatments that stimulate growth and mitigate the health side effects of dysplasias exist. There are mainly two kinds:
Surgical treatments to elongate the limbs.
Developmental treatments that try to go to the root of skeletal dysplasia by solving the hormonal disorders that modify normal bone growth.
Experts recommend a multidisciplinary approach to skeletal dysplasias as the best way to design SD treatmets.